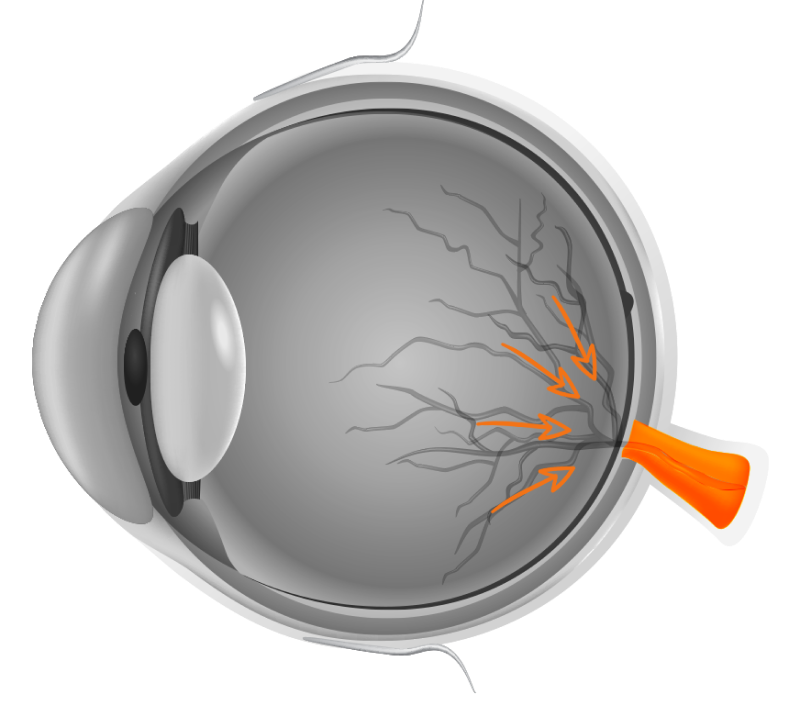
WHAT IS GLAUCOMA?
Glaucoma (Kala Motia) is a group of eye conditions wherein either the optic nerve or the retina gets severely damaged due to pressure caused by various factors. In most cases, glaucoma is painless but keeps getting worse over time and it gradually damages the peripheral vision and then the central vision, if left unaddressed it leads to complete blindness. On time diagnosis and appropriate treatment play an important role in treating glaucoma but ways of preventing glaucoma entirely is still a pending research.
TYPES OF GLAUCOMA
-
Open Angle Glaucoma: Elevated intraocular pressure and disc damage due to an increased resistance/blockage of the drainage pathway at a microscopic level (trabecular meshwork)
-
Angle-closure Glaucoma: Raised intraocular pressure and disc damage due to narrowing of the drainage system of the intraocular fluid.
-
Congenital Glaucoma: Present since birth. May or may not be associated with other systemic anomalies or syndromes.
-
Secondary Glaucoma: Caused due to injury to the eye, as side-effects of certain medications (topical or systemic), or sometimes surgery.
RISK FACTORS FOR GLAUCOMA
-
Age > 55 years, earlier if any positive family history is present
-
Family history of glaucoma
-
Taking corticosteroid medicines, especially eye drops, for a long time without a proper prescription from your doctor
-
Extreme near-sightedness (Myopia) or far-sightedness (Hypermetropia)
-
Black, Asian, or Hispanic race
-
Systemic risk factors: such as diabetes, migraines, high blood pressure and sickle cell anaemia, obstructive sleep apnoea
-
Thin corneas
-
Trauma to the eye
-
Post retina surgery
-
Some people have a narrow passage for the passage of water in the eye which puts them at an increased risk for angle-closure glaucoma
DIAGNOSIS OF GLAUCOMA
-
Applanation Tonometry: Measurement of the intraocular pressure. It is a small instrument mounted on the slit lamp which will touch the surface of the eye to measure the eye pressure. The eye is anesthetised before the procedure and a drop of fluorescein dye is instilled in the eye before the reading is taken. The surface of the tonometer is sanitised and sterilised after every use.
-
Gonioscopy: Inspecting the drainage angle or pathway. A special lens (gonioscopy lens) is placed on the surface of the eye along with a coupling fluid (liquid/gel) and then the Ophthalmologist examines the eye. The eye is anesthetised before the procedure and the lens is sanitised and sterilised after every use.
-
Pachymetry: Measuring corneal thickness. After anaesthetising the eye, a probe touches the surface of the eye for a few seconds and measures the corneal thickness. The probe is sanitised and sterilised after each use.
-
Optic Nerve Head photograph: a digital photograph of the optic nerve head is taken. It shows the physical changes on the nerve due to Glaucoma. Serial photographs can be used to observe the progression of the disease.
-
OCT (Optical Coherence Tomography): a computerised microscopic image of the optic nerve head. It measures the thickness of the nerve fibres and gauges the amount of damage (thinning) by comparing it with an age-matched database. It gives computerised, colourful printouts and serial scans that can be used for comparison and to assess the progression of the disease.
-
Perimetry or HVF/HFA (Humphrey Visual Fields / Humphrey Field Analysis): This is a comparatively larger machine. One eye is tested at a time. One or two tests are done per eye after placing your chin on the chin rest and after putting in the correct glass power. The patient has to press the trigger once he/she sees a flash of light. These flashes vary in brightness. This test is done in a dark room and while continuously looking at a fixation light within the machine. This test tests not only the patient’s field of vision but also sensitivity to bright and dim lights. This test is to be done in a calm and relaxed state of mind. The test may have to be repeated annually, biannually, or more frequently as required. Sequential test results can be used to detect the progression of the disease or the effectiveness of the current treatment in halting the progression of the disease, thereby helping to maintain vision.
TREATMENT OF GLAUCOMA
Glaucoma is treated by lowering intraocular pressure. Normal intraocular pressure is between 11-21 mm of Hg. Anything above 21 mm of Hg, warrants a complete eye examination to rule out Glaucoma. A person with intraocular pressure higher than normal but no signs of Glaucoma is labelled as having Ocular Hypertension. Sometimes Optic Nerve damage may occur when the IOP is within the normal range. This simply means that for that particular individual, even the normal range is high enough to cause nerve damage and he/she needs further lowering of intraocular pressure.
There are several treatment options for Glaucoma.
Eye Drops: Glaucoma treatment often starts with prescription eye drops. It works by decreasing the intraocular pressure by improving fluid drainage or decreasing the amount of fluid produced in the eye. Depending on how low your eye pressure needs to be, you may be prescribed one or more than one eye drop.
Oral Medications: Sometimes eye drops alone may not be sufficient to decrease your eye pressure enough so as to halt the progression of Glaucoma. Then your ophthalmologist may need to add oral medication.
Laser Treatment: is often used to try and enlarge the drainage passage, mostly in cases of angle closure glaucoma. Acute angle-closure glaucoma (where are angles of the eye are narrow and not draining fluid adequately) is a medical emergency. If you’re diagnosed with this condition, you’ll need urgent treatment to reduce the pressure in your eye.
You will be advised to undergo a procedure called a laser peripheral iridotomy. The doctor creates a small hole in your iris using a laser. This allows fluid to flow through the iris and helps to open the drainage angle of the eye and relieves eye pressure. In addition to this, eye drops and oral medications may be prescribed depending upon the reduction in IOP. This procedure however cannot be during the acute stage of the attack. The intraocular pressure needs to be lowered first.
-
Filtering surgery: This is a surgical procedure called a trabeculectomy (The ophthalmologist creates an opening/ alternate pathway in the white portion of the eye (sclera), for the intraocular fluid to drain, similar to a bypass. creates another space for fluid to leave the eye. Gonioscopy-assisted transluminal trabeculotomy (GATT) is a relatively newer, non-invasive technique, effective in lowering intraocular pressure in most cases.
-
Implants/ Drainage tubes: In this procedure, the eye surgeon inserts a small implant or tube in your eye to drain excess fluid to lower eye pressure.
Surgery: Surgery is mostly advised only if there is an inadequate lowering of intraocular pressure in spite of the patient being on Maximum Medical Therapy (MMT) or for some reason if the patient cannot continue with lifelong medical treatment. However regular follow-up is still required after the surgery.
After your procedure, you’ll need to see your eye doctor for follow-up exams. And you may eventually need to undergo additional procedures if your eye pressure begins to rise again or other changes occur in your eye.
PREVENTION
These steps may help detect and manage glaucoma in its early stages. That may help to prevent vision loss or slow its progress.
Get regular eye examinations:Regular comprehensive eye exams can help detect glaucoma in its early stages before significant damage occurs. As a general rule, the American Academy of Ophthalmology recommends a comprehensive eye exam every 5 to 10 years if you’re under 40 years old; every 2 to 4 years if you’re 40 to 54 years old; every 1 to 3 years if you’re 55 to 64 years old; and every 1 to 2 years if you’re older than 65.
If you’re at risk of glaucoma, you’ll need more frequent screening. Know your family’s eye health history. Glaucoma tends to run in families. If you’re at increased risk, you may need more frequent screening.
Wear protective eye gear:Serious eye injuries can lead to glaucoma. Wear eye protection when using power tools or playing sports.
Take prescribed eye drops regularly: Glaucoma eye drops can significantly reduce the risk that high eye pressure will progress to glaucoma. Use the eye drops as prescribed by your health care provider even if you have no symptoms.
Contact Us
A Unit of Shantilal Shanghvi Foundation
Copyright © JGDHealth. All Rights Reserved.