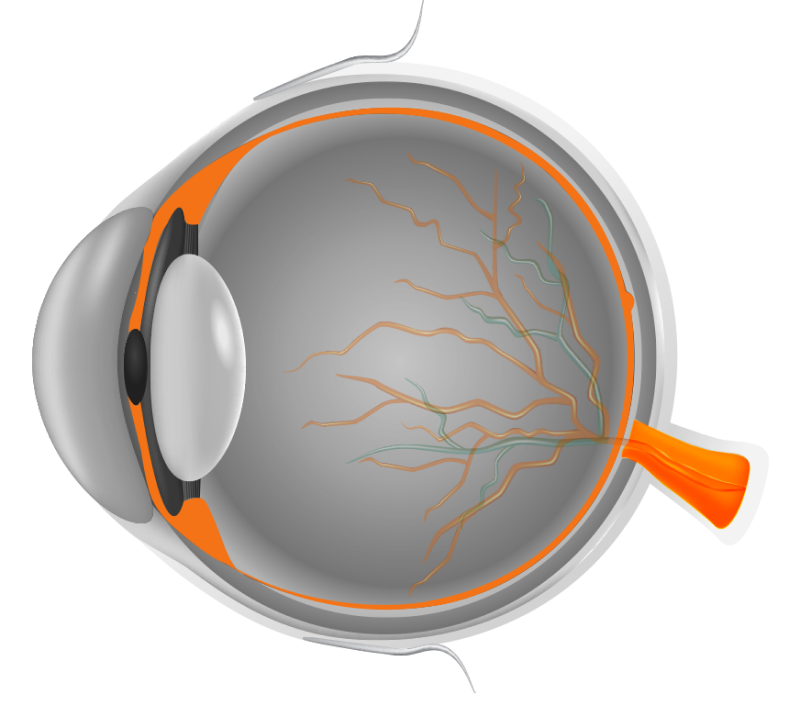
WHAT IS RETINA?
The retina is the innermost layer of the eye, which works like a camera film by capturing images and transferring them to the brain for processing and object perception. The area of the retina that controls your central vision is called the macula.
The retina is made up of ten layers, nine of which are in the neural retina and are supplemented by the outer pigment epithelial layer. The neural retina is made up of several layers of neurons. Of these, the photoreceptor layer is critical for detecting various light signals, which are relayed to the brain via the optic nerve.
To put it simply, the retina receives an image from the
focused light and sends it to the brain,
which then determines what the image is.
Diabetic Eye Care
What Is diabetic eye disease?
People with diabetes are at a higher risk of having certain eye diseases. Cataracts, diabetic retinopathy, and optic nerve disorders are among them. A common manifestation of diabetes in the eye is diabetic retinopathy (DR).
What is DR?
DR is primarily a disorder of the retinal blood vessels. Retinal blood vessel damage can result in vision loss or possibly blindness. Due to elevated blood sugar in people with diabetes, the cells that coat the blood vessels swell and are damaged. As a result, the blood vessels may leak fluid or bleed into the retina. Poor blood sugar management damages blood vessels to the point where they can block these, starving the retina of oxygen and nutrients.
Who can get DR?
Everybody with diabetes is at risk for eye problems, including retinopathy. Younger persons with diabetes may experience an earlier onset, and older people may experience a more gradual onset. Most people with diabetes will develop some degree of retinopathy after ten years of the disease.
What is Diabetic Macular Edema (DME)?
DME is an accumulation of fluid (edema) in the macula, the central part of the retina, responsible for critical seeing needs like reading, identifying faces, and driving. DME is the major cause of vision loss in people with DR. It can happen at any stage of the disease; however, it is more likely as diabetic retinopathy gets worse.
What are the symptoms of DR and DME?
Typically, DR does not show any symptoms in its early stages. The illness frequently advances silently until it starts to impact vision. Vision blurring may result from DME. Bleeding from the damaged retinal blood vessels can cause “floating” spots to appear. Sometimes, these patches disappear on their own. However, if bleeding is left untreated, it frequently returns, raising the possibility of permanent vision loss.
How to detect DR and DME?
A thorough dilated eye exam that includes the following can identify DR and DME:
- Vision testing for distance and near.
- Pupil dilation for detailed retinal evaluation: Changes in the lens and blood vessels, leakage or bleeding from the blood vessels, and swelling in the retina.
- Optical coherence tomography (OCT).
- Fluorescein angiography may be performed if DME or severe DR is suspected to search for damaged or leaking blood vessels.
How are DR and DME treated?
Treatment goals for DR and DME include:
- Restoration of vision
- Stabilize the disease
- Slow down the disease progression
Treatments Include:
Intravitreal Injections – These medications are injected inside the eye to reduce the swelling in the retina, prevent further leakage from the blood vessels, and cause faster resolution of the bleeding inside the eye.
Laser Therapy –A laser beam is used to seal off or obliterate leaky vessels.
Vitreous Surgery –Some cases of advanced disease may not respond to treatment, despite injections and laser therapy. Vitreous surgery may be indicated in these patients.
What Can I do to reduce the risk of DR and DME?
- Maintain blood sugar and HbA1C levels within the desired range
- Control your blood cholesterol and blood pressure
- Avoid smoking
- To keep a healthy body weight, eat nutritious meals, limit your portions, and exercise frequently
- Take the medication regularly as prescribed by your doctor
Are any specific things I should keep in mind during my diabetic eye care?
- Diabetes retinopathy is a chronic, progressive disorder. The risk of vision loss due to diabetic retinopathy can be decreased but not eliminated by injections/laser/surgery. A periodical check-up is required to detect any worsening retinopathy and to provide suitable treatment.
- The risk of DR progression and vision loss worsens with uncontrolled diabetes
- Because diabetes affects multiple systems, continuous care from your doctor is crucial.
Retinal vein occlusion (RVO)
What is RVO?
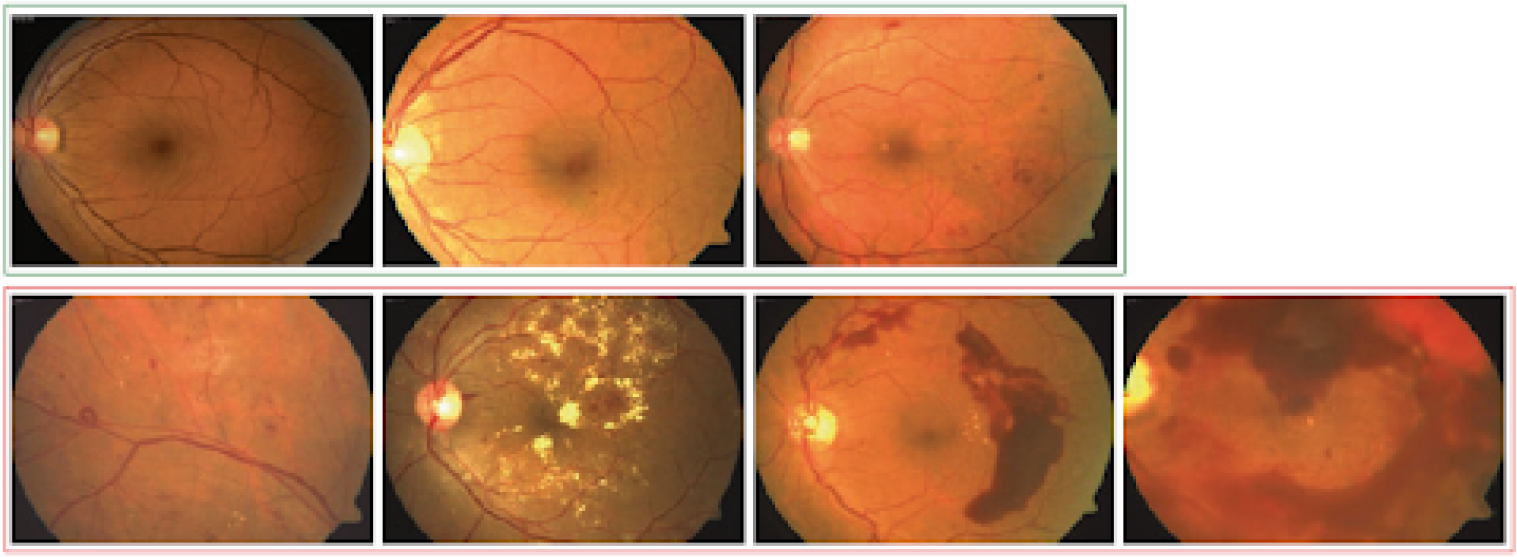
In RVO, there is blockage of the small blood vessels which drain the blood from the retina. It is commonly seen in people with hypertension and diabetes. It is characterized by multiple bleeding spots within the retina. Many people may have decreased vision due to fluid accumulation within the retina (edema).
How do we diagnose RVO?
RVO can be diagnosed clinically. The optical coherence tomography (OCT) scan is beneficial for scanning the retina and identifying any retinal edema. A fundus fluorescein angiography (FFA) may be performed to determine the degree of blockage within the retina.
How do we treat RVO?
Intravitreal injection – The first line of treatment for retinal edema due to RVO is intravitreal injections. Multiple injections may be needed for the best visual outcomes.
Laser – Retinal laser is required to areas outside the macula to decrease the stimuli (areas of capillary non-perfusion) and the growth of abnormal vessels.
Vitreous surgery – Despite treatment or due to inadequate response to treatment, there could be bleeding inside the eye. Many eyes with bleeding inside the eye due to RVO would need vitreous surgery.
Retinal Detachment (RD)
Normally the retina is firmly attached to the back of the eyeball. If it becomes detached, the eye loses vision. This is a rare disease occurring in about one person out of 10,000, each year. The immediate cause is usually a hole in the retina. It may be due to injury or surgery but is usually due to weakness of the retina. This is sometimes called retinal degeneration. Retinal detachment is commonly managed surgically, either by scleral buckling (SB) or pars plana vitrectomy (PPV), or a combination of both.
Prevention of Retinal detachment:
In some cases, the retina is more fragile and prone to the formation of holes or breaks. If these are detected and sealed in the early stages by laser or cryosurgery, retinal detachment can be prevented. People who are likely to develop retinal detachment should have periodic examinations done after dilation of the pupils. Some of the situations where this is desirable are:
- History of detachment in one eye
- Family history of retinal detachment
- History of injury to the eye or its surrounding bones
- History of flashes and floaters
- Sudden onset of floaters or change in the character of floaters
Retinopathy of Prematurity
Eyes of a premature baby?
The inside of the eye, the retina is not fully developed in premature babies. Abnormal blood vessels can develop in such a retina. These abnormal blood vessels can cause internal bleeding and even retinal detachment. This is called Retinopathy of Prematurity (ROP). This condition results in low vision or blindness – both of which are irreversible.
How to detect ROP?
A trained ophthalmologist can detect ROP by dilating the pupils of the eye using eye drops. An indirect ophthalmoscope is used to scan the entire retina to detect ROP and gauge the state of retinal maturity.
What are the indication for retinal examination for ROP in new babies?
- Babies with a birth weight of less than 2000 grams or those born in under 34 weeks of pregnancy are most likely to have ROP.
- Pre-term babies who have had problems after birth such as lack of Oxygen, infections, blood transfusions breathing trouble, etc., are also vulnerable.
- Follow the “Day-30” strategy. The retinal examination should be completed before “day-30” of the life of a premature baby. It should preferably be done earlier (at 2-3 weeks of birth) in very low weight babies (<1200 grams birth weight).
What are the treatment options for ROP?
ROP is treated with Laser rays /Injections (Anti VEGF)/surgery /combination. The treatment helps stop further growth of abnormal vessels thus preventing vision loss.
How frequently should be the retinal evaluation done for babies with ROP?
ROP can progress in 7-14 days and therefore, needs a close
follow-up till the retina matures.
Need for urgent treatment in ROP. It needs to be treated as soon
as it reaches a critical stage called Threshold ROP. There is
50% or greater risk of vision loss if left untreated after this.
Time is crucial. If treated in time, the child is expected to
have reasonably good vision. All premature babies need regular
eye examinations till they start going to school. They may need
glasses or treatment for lazy eyes/ cross-eyes and sometimes,
for cataract, glaucoma and retinal detachment.
What are the investigations available at Shantilal Shanghvi Eye Institue?
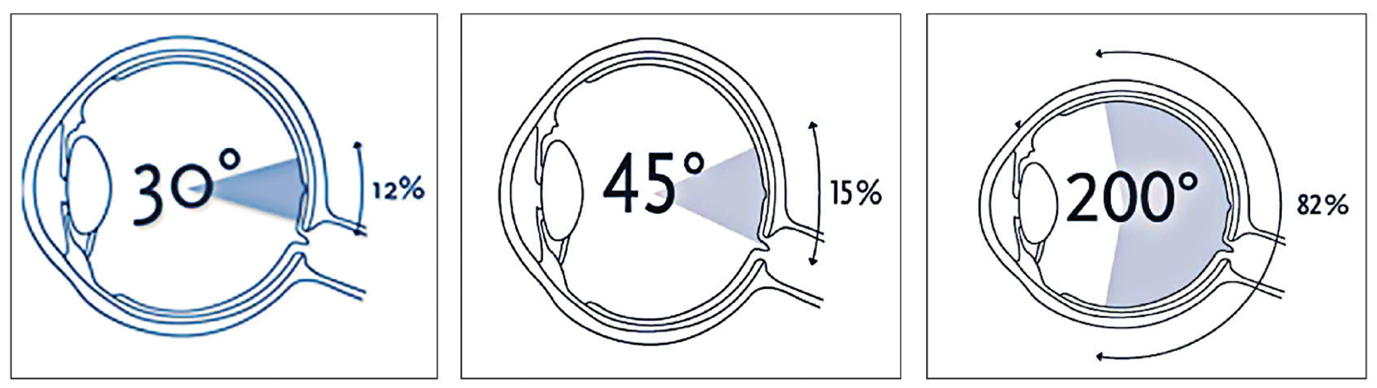
Ultra-widefield Color fundus photography (CFP) – It involves capturing the photograph of the retina and the nerve in one go. The normal CFP captures a 30-50 degrees field of view of the retina. The ultra-widefield camera captures a 200 degrees field of view, which helps visualize around 80% of the retina.
Fundus Autofluorescence (FAF): A specialized non-invasive imaging test that utilizes light of longer wavelength to examine the outermost layer of the retina known as the retinal pigment epithelium (RPE).
Optical coherence tomography (OCT): It is a light-based scan of the retina and the nerve, which provides detailed cross-sectional images of the tissues.
Fundus fluorescein angiography (FFA): Sodium fluorescein dye is injected into the blood circulation, usually through an arm vein, in this test. The retina is photographed as the dye enters the eye. It gives us an insight into the damage to the blood vessels of the retina.
Indocyanine green angiography (ICGA): This angiography uses a special dye called Indocyanine green for a detailed evaluation of the layer outside the retina, known as choroid. The choroid is important as it nourishes the outer layers of the retina.
Optical coherence tomography angiography (OCTA): In the investigation, the normal and abnormal blood vessels are visualized without injecting any dye.
B-scan ultrasonography: This is a sonography test that utilizes sound waves to examine the interior of the eye. It is useful to evaluate the eye and the globe when it is not possible with routine clinical examination.
What are the treatment options for Vitreoretinal diseases?
Intravitreal injections: These medications must be injected directly into the eye for an adequate drug concentration to reach the retina. A few common indications for injections include DR (macular edema, wet ARMD, RVO, and infection inside the eye (endophthalmitis). It is a day-care procedure that is painless. It is done after instilling a few numbing (anaesthetic eye drops). You will be discharged immediately and can resume working the next day.
Laser treatment: In laser therapy, a specific beam of light is directed onto the damaged retina without injuring the surrounding tissues. The goal is to either seal any leaks or retinal breaks or obliterate the damaged retina. Depending on the disease condition, the treatment might take anywhere from 10 to 30 minutes. Most patients report no pain, while some may experience a minor headache and eye discomfort. At SSEI, we have a specialized multi-spot laser that can deliver 25 laser spots in one go. This considerably reduces the duration of the laser therapy and makes the procedure extremely comfortable. The common indications for laser treatment include DR, RVO, ROP, CSCR, and retinal breaks.
Vitrectomy Surgery: In this surgery, most of the non-transparent vitreous is removed and replaced with a clear solution. Vitrectomy is usually done to remove the pulling forces of the vitreous over the retina which would have led to various retinal pathologies. Patients with retinal detachment may require additional tamponades like gas or silicone oil whereas macular hole surgeries need gas tamponade. Sometimes it is done for diagnostic purposes for diseases of unknown origin. Occasionally it may be necessary to inject air, gas, or silicone oil into the eye after removing the vitreous gel.
Contact Us
A Unit of Shantilal Shanghvi Foundation
Copyright © JGDHealth. All Rights Reserved.